By Kate Mulligan, Assistant Professor, Social & Behavioural Health Sciences, Dalla Lana School of Public Health, University of Toronto
The Omicron wave seemed to come like a rising tide, slowly, then suddenly, in all directions and all at once. Inside the health-care system, skeleton crews face impossible workloads and moral distress.
Outside of it, people are feeling the weight of things like deferred care, deprioritized essential workers, online learning and doomscrolling. People are sick not just with COVID-19, but with isolation, inequity and polarization. So it should not be a surprise if the recent announcements of shuttered schools and renewed restrictions have some people feeling it’s all just too much to sustain.
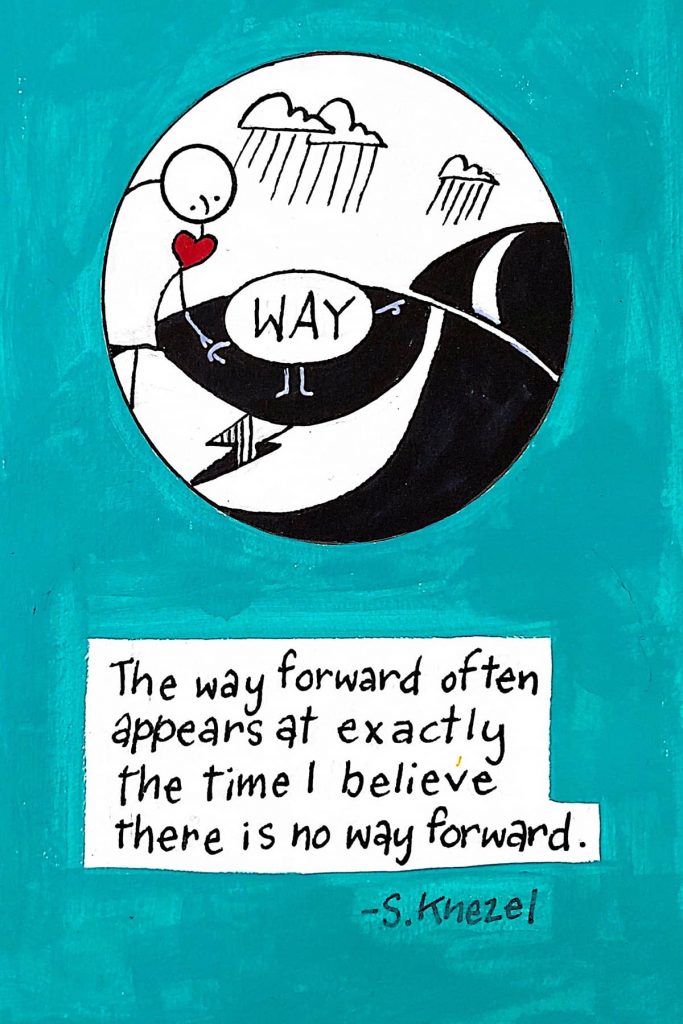
But there is a way through difficult stages of the pandemic. It is possible to counter helplessness and build power by creating a sense of purpose and community amidst the confusion of COVID-19.
Self-determination
As a researcher of social prescribing — the act of using health-care visits as a starting point to reconnect people with health-promoting community services — I want to share some steps we can all take today to get back to the basics of health promotion, using self-determination to help exert more control over our own individual and shared experiences.
Self-determination is a widely used approach in health promotion that derives from two distinct bodies of research: in psychology, about how we build well-being in our own lives, and in political science, about how together we govern the things that are most important to us. The idea, in both traditions, is that by applying just four principles at individual and collective levels, people can increase control over and improve the conditions for their health and well-being.
Autonomy
First, there is a need to rediscover autonomy: the ability to make decisions for yourself. When it feels like so much control has been taken away, making a small decision of your own can help you shift from worrying about “what’s the matter with me” to taking action on “what matters to me.”
In social prescribing, participants don’t wait for someone else to make a treatment plan. They voice their own well-being priorities and are supported to take more control over their own health goals. This can start with something as small, but healthful, as picking up a drawing pencil or going for a walk in nature, or something more intensive like accessing support for housing or volunteering with others in your community.
Politically and at the community level, fostering autonomy can look like ensuring people have support to make local economic decisions, supporting local public health and community organizations, or ensuring vaccine outreach is both scientifically accurate and culturally meaningful.
Competence
Next, we need to value competence: our ability to influence outcomes and to show ourselves and others what we are capable of. During times of collective crisis, people can feel powerless in the face of forces larger than themselves. In social prescribing, participants are supported to get back in touch with their own power, focusing less on what they can’t do and more on what they can, by doing something they’re good at.
For communities, valuing competence can mean taking a strengths-based or asset-based approach that recognizes the unique capacity and expertise within a community — such as trusted relationships, local ecological knowledge and under-recognized training — rather than focusing on community deficits.
Beneficence
Closely related to a sense of competence is finding beneficence: the sense of having a positive impact on others. There is a demonstrable giver’s glow that comes from helping; regardless of individual constellations of ability, health and privilege, everyone has something to give.
In social prescribing, participants who express a desire to give back are supported to take the lead in volunteering to help others or designing and implementing new programs and services. At a broader level, fostering collective beneficence might look like prosocial communications approaches that remind us of how COVID-19 precautions help others, or opportunities to help others access vaccines and supports.
Relatedness
Finally, we need to value relatedness: the sense of connection and belonging with others and the world around us. Feelings of loneliness and social isolation have grown during the COVID-19 pandemic, with significant impacts on health and well-being.
In social prescribing, participants are afforded the time and space to develop relationships: with a community connector who listens, with friends and family, or with other participants who may have something in common.
Collectively and politically, recognizing relatedness can look like supporting policies that accommodate people as both workers and carers, ensuring the shared protection of global vaccine equity or taking action on the ecological and climate pressures that increase the risk of zoonotic diseases.
Self-determination means deciding for ourselves, feeling proud of a job well done, giving to others and feeling we belong. Social prescribing can’t be everything to everyone, but what it has shown is individual and collective well-being, psychological and political self-determination are deeply intertwined.
Starting with one phone call, walk in the park, poem or gift does make a difference, and can help kick-start the ability to get through these challenging times — together.
Nаthаn Dеnеttе, Frаnk Gunn, and Grеgorіо Bоrgіа
Originally published on The Conversation as Feeling powerless in the COVID-19 pandemic? 4 principles of self-determination can help you take back some control
Support evidence-based journalism with a tax-deductible donation today, make a contribution to The Conversation.