Elisa Reyes has come to Plaza del Sol Family Health Center for doctor’s appointments for more than a decade. She moved away a while ago but keeps returning, even if it means a two-hour roundtrip bus ride.
That is because her two children see the same doctor she does. Because when she is sick, she can walk in without an appointment. Because the staff at the Queens clinic helped her apply for health insurance and food stamps.
“I feel at home. They also speak my language,” Reyes, 33, said in Spanish. “I feel comfortable.”
Plaza del Sol is one of two dozen sites run by Urban Health Plan Inc., which is one of nearly 1,400 federally designated community health centers. One in 11 Americans rely on these to get routine medical care, social services and, in some cases, fresh food.
The clinics serve as a critical safety net in every state and U.S. territory for low-income people of all ages. But it is a safety net under stress.
Since 2012, community health centers have seen a 45% increase in the number of people seeking care — and they have opened more and more service sites to expand their footprint to more than 15,000 locations.
Many centers are short-staffed and struggling to compete for doctors, mental health professionals, nurses, and dentists. Leaders also said that funding is an ever-present concern, with the months-long debate over the federal budget making it all but impossible for them to plan and hire for the long term.
Community health centers have been around in some form for decades, and are largely what remains when urban and rural hospitals close or cut back on services.
Dr. Matthew Kusher, Plaza del Sol’s clinical director, said there are things that prescriptions cannot change, like stopping the spread of flu and COVID-19 when people live in apartments with one family per room and it is impossible to quarantine.
“What we provide here is only 20% of what goes toward somebody’s health,” Kusher said. “Their health is more driven by the other factors, more driven by the poverty, and the lack of access to food or clean water or healthy air.”
Nine in 10 health center patients live at or below 200% of the federal poverty line, according to the U.S. Health Resources and Services Administration. Beyond that, in 2022 nearly 1.4, one in five was uninsured, and half were on Medicaid.
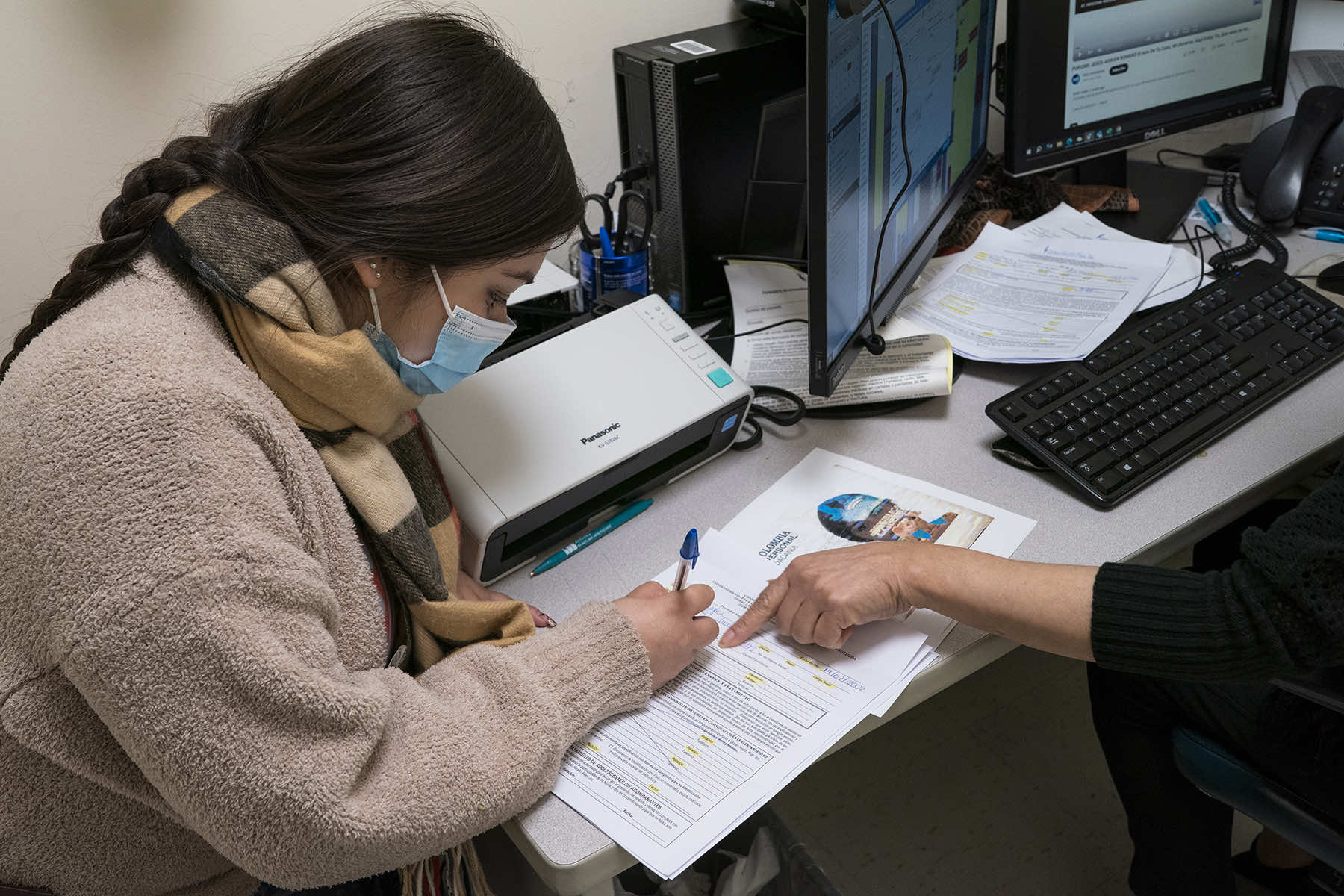
One in four was best served in a language other than English; about 63% were racial or ethnic minorities.
Dr. Acklema Mohammad started 50 years ago as a medical assistant in Urban Health Plan’s first clinic, San Juan Health Center. She has cared for some families across three generations.
“It’s so gratifying to work in this community. I’m walking through the door, or I’m walking down the street, and I’m getting hugs,” she said. “All along, ‘Oh, Dr. Mo! You’re still here!'”
Staffing is Mohammad’s biggest worry. Many pediatricians retired or left for other jobs after the worst of the pandemic. It is not just about money, either: She said job applicants tell her they want quality of life and flexibility.
“It’s a big job and it’s a big issue because we have so many sick children and so many sick patients,” Mohammad said, “but we don’t have enough providers to take care of them.”
Former pediatricians are sometimes picking up virtual visits to provide relief, she said, and telehealth helps, too. But when telehealth is not a possibility, El Nuevo San Juan Health Center tries to bring care to people instead.
About 150 elders get at-home visits, said Dr. Manuel Vazquez, Urban Health Plan’s vice president of medical affairs who oversees the program. There are times when the care is not covered, but the team does it without pay.
“We said, ‘No. We need to do this,'” he said.
BUILDING COMMUNITY TRUST
One of the nation’s first community health centers opened in the rural Mississippi delta in 1967, in the wake of the Civil Rights Movement’s Freedom Summer.
Today, Delta Health Center in Mound Bayou, Mississippi, has 17 locations in five counties, including free-standing clinics and some in schools.
Access to preventive care is critical as area hospitals cut back on neonatal services and other specialty care, said Temika Simmons, Delta Health Center’s chief public affairs officer.
“If you’re in the middle of a heart attack, you’re going to have to be airlifted to Jackson or Memphis where they have the equipment to save your life, and so you might die along the way,” she said. “So, what we’ve been doing in terms of primary care is trying to keep people away from that part.”
Another key to the centers’ ability to improve health disparities is understanding and being part of their communities. Plaza del Sol is located in the heavily immigrant, mostly Latino neighborhood of Corona, which was the epicenter of New York City’s COVID-19 spread. Staff are required to speak Spanish.
The Mississippi Delta staffers are trained to spot signs of abuse, Simmons said, or know that the patient “fussing and fighting” about filling out a form likely cannot read.
To continue to serve the communities in the way they want to, center leaders say they are stretching dollars are far as they can — but need more.
Based on the rising number of patients and inflation in the health care sector, federal funding for centers would need to increase by $2.1 billion to match 2015 funding levels, according to an analysis sponsored by the National Association of Community Health Centers.
“You can’t be overwhelmed with the problem,” Simmons said. “You’ve got to just simply take it one day at a time, one patient at a time.”