Health care workers scrambled to treat patients on a day when 92 Wisconsin lives were reported lost. Outside of the hospital, politicians postured.
The exterior of University Hospital in Madison on November 17 looked remarkably ordinary. A line of cars queued outside of the parking garage, where drivers must still push a button and grab a ticket before entering. Patients streamed in and out of the building. The first hint that these are extraordinary times: everyone wore masks as screeners checked visitors’ symptoms and temperatures.
Parts of the COVID-19 unit three floors upstairs also looked unspectacular. The floor was designed for general care — a little bit of everything — when a pandemic isn’t raging. But November 17 marked one year since the coronavirus was first detected in China, beginning its destructive journey around the world.
Wisconsin reported on November 17 a single-day record 92 deaths linked to the virus, pushing the state’s full pandemic death count to 2,741. (State officials have since reported 135 additional deaths in two days.) Some 2,277 COVID-19 patients filled 89% of the state’s available hospital beds. Of those patients, 177 were in Dane County, home to University Hospital.
The hospital currently has five COVID units, plus another unit in a facility across town. The hospital repurposed this unit in March when it started admitting significant numbers of coronavirus-infected patients. Negative air pressure in each room prevents the virus from drifting into the hallway. Patients are now consistently filling all 28 of the unit’s beds, said Mary Lowe, a nursing assistant who has worked in the unit since 2019.
She recalls seeing patients as young as 20 years and as old as 91.
The unit was often busy before the pandemic, she said, but these days, she often feels overwhelmed. These patients are severely ill. Lowe’s work brings her in direct contact with seven or eight COVID patients a day, helping them with everything from eating to using the restroom and bathing. She tries to minimize the number of visits to each room — to protect herself and preserve scarce protective gear. That means doing more with each visit.
“There’s just so much to do,” said Lowe.
Counterintuitively, Lowe said she feels safer inside the hospital than she does outside. She knows exactly what she’s dealing with here — who has COVID and who doesn’t. The protective gear helps, too. In that sense, the ward feels like the calm eye of a hurricane.
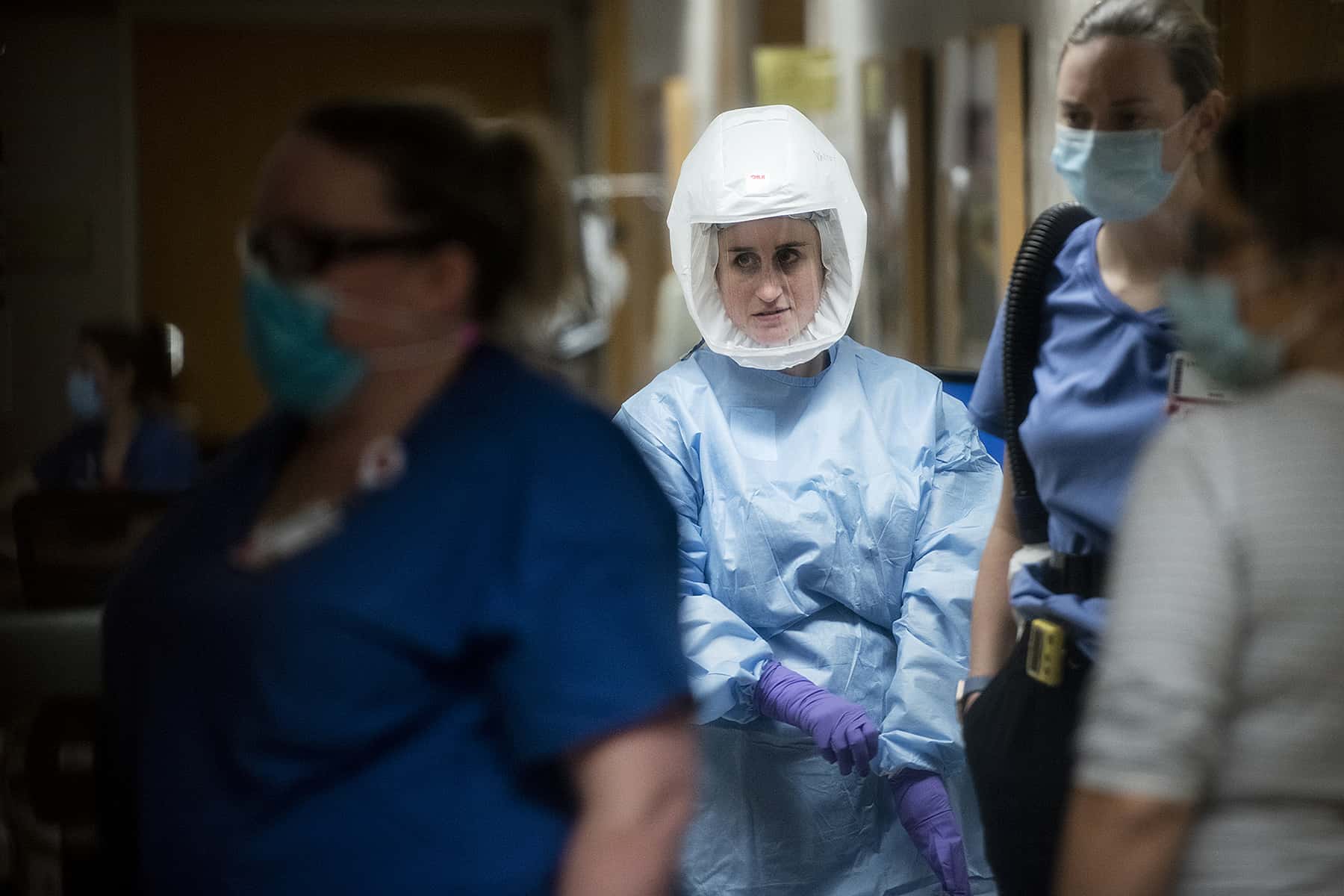
Medical staff walking the halls wear surgical masks. They suit up in full protective gear before entering each patient’s rooms: gown, gloves and facial protection. Lowe recently transitioned from using an N95 mask and face shield to wearing an air-purifying respirator called a PAPR. It resembles a soft astronaut’s helmet, and a tube connects to an air filter that a belt holds in place at her waist. Lowe likes that a PAPR allows patients to see her face. They know when she’s smiling, and hard-of-hearing patients can read her lips.
The hospital’s other COVID units treat the most serious patients — those who are unconscious and on a ventilator. By contrast, Lowe’s patients are generally alert, usually getting oxygen, steroids and personal care.
Lowe gets to know them. She also offers emotional support, considering that no visitors are allowed except on a very limited basis and only near the end of a patient’s life. Among the hardest times: when patients leave to receive more intensive care in another unit. Those are the folks who may not recover.
“Patients are suffering,” Lowe said. “People are really sick here. We’re all working really hard to help them get better and to support them. But it’s definitely straining us.”
That is why the hospital is allowing reporters to peer inside this COVID unit. It’s why Lowe is taking time eight hours into her 12-hour shift to talk. Treating COVID patients is exhausting month after month. Even with the promising news about vaccines, health care workers see no end in sight.
Outside the hospital on November 17, infections continued to surge in Wisconsin, where fiercely partisan politics and viral misinformation have paralyzed the state’s response to the pandemic and muddled messaging about ways to slow the infections and deaths: Wear a mask. Keep a distance. Wash your hands.
Assembly Speaker Robin Vos, R-Rochester, held a press conference to unveil “new COVID initiatives.” After the press conference was announced, Governor Tony Evers, a Democrat, unveiled a draft of his own $541 million package to address the pandemic’s damage to public health and the economy. It includes measures to streamline processing of jobless claims — alongside an evictions moratorium and requirements that insurers cover COVID-19 testing, treatment, prescriptions and vaccines. Governor Evers shared the legislation with GOP leaders a night earlier, his office said, but he did not immediately hear back.
Vos and the Republican party controls both chambers of a Legislature that has not passed a bill since April. His colleagues have drafted no legislation, he told reporters November 17, suggesting they might find some common ground with Governor Evers. Vos expressed interest in expanding ranks of contact tracers, aiding small businesses and improving testing. But incoming Senate President Chris Kapenga, R-Delafield, later said that he saw no reason for legislative action.
Evers has sought to limit gatherings and pursue other restrictions to slow the virus’ spread, drawing resistance from Republicans and business groups at every step. Courts have thwarted Evers’ Safer at Home order and a subsequent order to limit bar and restaurant capacity. The Wisconsin Supreme Court is weighing an additional challenge to Evers’ mask-wearing mandate.
Meanwhile the Wisconsin Department of Health Services reported more than 7,000 new infections during Lowe’s shift on November 17, with 318 additional COVID patients checking into hospitals — another daily record. And as Thanksgiving looms, Evers, DHS Secretary-designee Andrea Palm and the federal Centers for Disease Control and Prevention are all warning that even small gatherings could lead to even more sickness and death.
“Our hospitalization rate continues to look like a mountain, and we’re still climbing that mountain,” said Dr. Ann Sheehy as she stood in a University Hospital COVID unit hallway that whirred like a wind tunnel.
“We really need help from the people of Wisconsin to help us shut this down,” Sheehy said. “There’s nothing more we can do as health care providers, without the help of the community at this point. It’s really up to them as to how bad things are going to get inside the walls of the hospital.”
As head of the division of hospital medicine, Sheehy manages staffing and scheduling care for COVID patients — while offering care herself. Among her biggest concerns: Her colleagues are tired as they juggle intense daily work along with the more personal stresses of the pandemic. Clinicians have families at home. Their kids are home from shuttered schools, learning remotely. Their routines are upended, and they have few options to alleviate stress.
“This is a group that’s really driven to take good care of patients and will continue to go above and beyond until they just can’t,” Sheehy said.
That is what she wants Wisconsinites to know. Doctors and nurses and other hospital staff are working as hard as they can to keep residents alive during this pandemic. But at a certain point, they need everyone else to pitch in — and help slow the spread of this horrible disease.
Peter Cameron
Coburn Dukehart and Will Cioci
The nonprofit Wisconsin Center for Investigative Journalism collaborates with Wisconsin Public Radio, Wisconsin Public Television, other news media and the UW-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by the Center do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.




















